Scientific breakthroughs in one disease don’t always shed light on treating other diseases.
But that’s been the surprising journey of one Mayo Clinic research team in the United States.
After identifying a sugar molecule that cancer cells use on their surfaces to hide from the immune system, the researchers have found that the same molecule may eventually help in the treatment of type 1 diabetes.
Once known as juvenile diabetes, type 1 diabetes is a chronic autoimmune condition in which the immune system errantly attacks the pancreatic beta cells that produce insulin.
The disease is caused by genetic and other factors.
In their studies, the researchers took a cancer mechanism and turned it on its head.
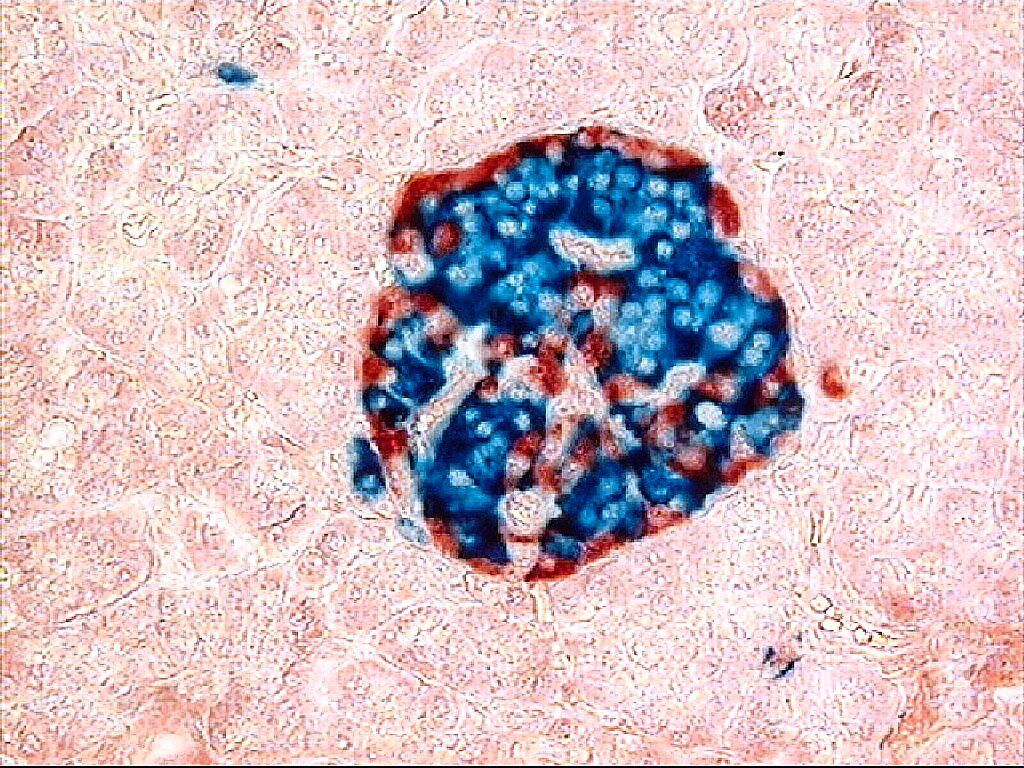
Cancer cells use a variety of methods to evade immune response, including coating themselves in a sugar molecule known as sialic acid.
The researchers found in a preclinical model of type 1 diabetes that it’s possible to dress up beta cells with the same sugar molecule, enabling the immune system to tolerate the cells.
“Our findings show that it’s possible to engineer beta cells that do not prompt an immune response,” says study principal investigator and immunology researcher Dr Virginia Shapiro.
A few years ago, Dr Shapiro’s team demonstrated that an enzyme, known as ST8Sia6, which increases sialic acid on the surface of tumour cells, helps these cells appear as though they are not foreign entities to be targeted by the immune system.
“The expression of this enzyme basically ‘sugar coats’ cancer cells and can help protect an abnormal cell from a normal immune response.
“We wondered if the same enzyme might also protect a normal cell from an abnormal immune response,” she says.
The team first established proof-of-concept in an artificially induced model of diabetes.
In the current study, published in the Journal of Clinical Investigation, the team looked at preclinical models that are known for the spontaneous development of autoimmune (type 1) diabetes, most closely approximating the process that occurs in patients.
Researchers engineered beta cells in the models to produce the ST8Sia6 enzyme.
In the preclinical models, the team found that the engineered cells were 90% effective in preventing the development of type 1 diabetes.
The beta cells that are typically destroyed by the immune system in the disease were preserved.
Importantly, the researchers also found that the immune response to the engineered cells appears to be highly specific, says study first author and Mayo Clinic Alix School of Medicine and Mayo Clinic Graduate School of Biomedical Sciences MD-PhD student Justin Choe.
“Though the beta cells were spared, the immune system remained intact,” he says.
The researchers were able to see active immune B- and T-cells, and evidence of an autoimmune response against another disease process.
“We found that the enzyme specifically generated tolerance against autoimmune rejection of the beta cell, providing local and quite specific protection against type 1 diabetes.”
No cure currently exists for type 1 diabetes, and treatment involves using synthetic insulin to regulate blood sugar, or for some people, undergoing a transplant of pancreatic islet cells, which include the much-needed beta cells.
Because transplantation involves immunosuppression of the entire immune system, Dr Shapiro aims to explore using the engineered beta cells in transplantable islet cells with the goal of ultimately improving therapy for patients.
“A goal would be to provide transplantable cells without the need for immunosuppression,” she says.
“Though we’re still in the early stages, this study may be one step toward improving care.”
The research was funded by grants from the US National Institutes of Health. – Mayo Clinic News Network/Tribune News Service





