The frequency of prostate cancer is rising rapidly and is expected to double within the next 10 to 15 years.
In 2020, there were approximately 1.4 million new cases worldwide, with 375,000 deaths annually.
By 2040, the World Health Organization (WHO) predicts there will be nearly 2.9 million cases and 750,000 deaths each year.
This alarming trend is considered unavoidable.
Unlike many other cancers, prostate cancer cannot be prevented by lifestyle modifications alone, nor can it be significantly reduced through conventional public health measures.
What we can do, however, is place greater emphasis on education, awareness and early detection.
These steps are especially important in identifying and treating lethal localised prostate cancers before they spread.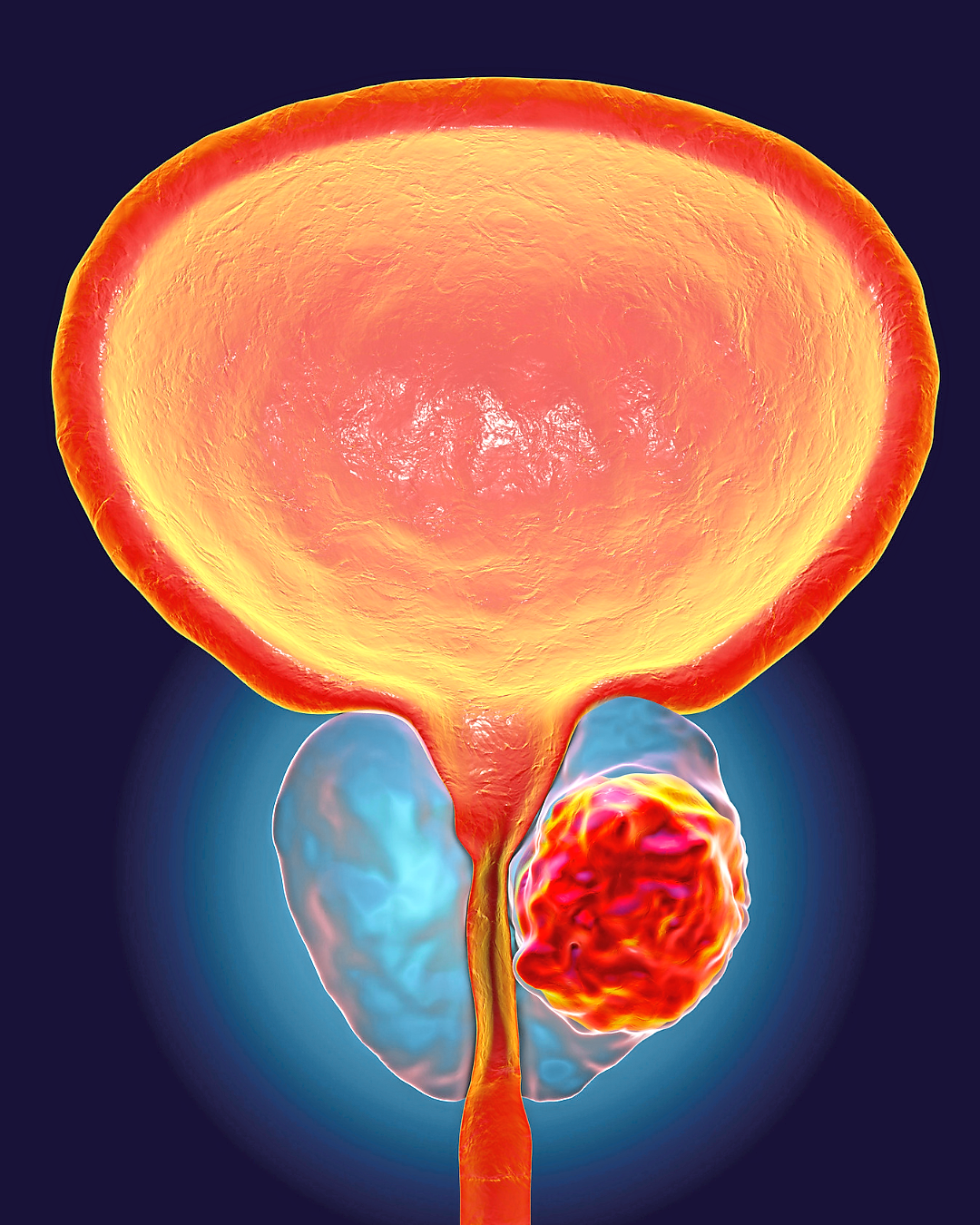
Is screening still controversial?
In previous decades, prostate cancer screening was controversial, largely due to concerns about “overdiagnosis” and “overtreatment”.
Today, this issue is becoming far less relevant.
In many developing countries, the bigger challenge is underdiagnosis.
Too many men are never screened until it is too late.
Every clinically significant prostate cancer has the potential to cause harm, and every cancer begins as a small lesion before growing into a life-threatening disease.
Early detection, therefore, remains crucial.
Thanks to advances in technology – such as high-resolution imaging and precision diagnostic tests – physicians can now classify prostate cancer more accurately into low-, intermediate- and high-risk categories.
This enables tailored treatment strategies, ensuring men receive the right level of care without unnecessary intervention.
One of the most important insights in modern urology is that not all prostate cancers are inherently life-threatening.
Many are slow-growing and may never cause harm during a man’s lifetime.
For such cases, deferring treatment is not dangerous, provided the cancer is correctly identified and carefully monitored.
This paradigm shift has allowed doctors to counsel patients more effectively and consider individualised treatment plans, rather than defaulting to aggressive, whole-gland therapies.
Better diagnostic tools
The management of localised prostate cancer has changed dramatically over the past two decades.
The single greatest breakthrough has been the introduction of multiparametric MRI (mpMRI).
mpMRI provides unparalleled detail by:
> Identifying suspicious lesions
> Measuring water movement within tissue (Diffusion-Weighted Imaging [DWI])
> Assessing blood flow patterns (Dynamic Contrast Enhancement [DCE]).
With mpMRI, doctors can:
> Avoid unnecessary biopsies in around 30% of men > Improve the detection of aggressive cancers
> Perform MRI-guided fusion biopsies for highly accurate sampling of suspicious regions.
This transformative precision diagnostic technique has become well established over the past five years, allowing prostate cancer to be diagnosed and graded more reliably than ever before.
Traditional treatments
Historically, the two main treatments for localised prostate cancer were radical prostatectomy (surgical removal of the prostate) and radiotherapy (radiation directed at the prostate).
While both approaches are effective in controlling disease, they are also associated with significant side effects such as:
> Erectile dysfunction (mainly from surgery initially)
> Urinary incontinence (mainly from surgery)
> Bowel toxicity (from radiotherapy)
> Radiation cystitis and bladder complications
> Surgical risks, including blood loss, hospitalisation and post-operative complications.
Urinary incontinence occurs in up to 40% of men undergoing radical prostatectomy, although permanent incontinence affects only about 5% in medical centres of excellence.
Erectile dysfunction and ejaculatory disorders occur in 70-90% of cases, even with the best surgical expertise.
Understandably, many men hesitate to pursue treatments that so profoundly affect their quality of life.
More focused treatment
For the majority of men, focal therapy provides a promising “middle ground”.
Instead of removing or irradiating the entire prostate, focal therapy targets only the cancerous area while preserving the remainder of the gland.
Using high-intensity focused ultrasound (Hifu), bursts of sound waves are directed with pinpoint precision to ablate cancerous tissue while sparing surrounding structures.
Key advantages of focal therapy include:
> Preserving vital structures such as the bladder, rectum, nerves and urinary sphincter
> Reducing the risk of incontinence and erectile dysfunction
> Keeping future treatment options open
> Maintaining quality of life.
For men with low- or intermediate-grade cancers (which account for 80–85% of localised cases), focal therapy is often the most appropriate option.
Only about 15% of prostate cancers are aggressive enough to require radical whole-gland treatment.
Candidates for focal therapy must be:
> Carefully assessed based on tumour size, location and grade
> Fully informed of the risks and benefits of partial-gland treatment
> Committed to regular follow-up appointments and surveillance.
Compliance with follow-up is essential, as focal therapy depends on early recognition of recurrence or progression.
Pros and cons
Current evidence shows encouraging cancer control rates at five years across all major treatment methods:
> Surgery: 90-95%
> Radiotherapy: 70-90%
> Focal therapy: 80-85%.
What makes focal therapy especially attractive is that it offers comparable cancer control in selected patients, while significantly reducing side effects that impair daily living.
Multiple large clinical studies and trials in Europe and the United States confirm these results.
Notably, the FARP study in Norway, which reported its results last year, supports focal therapy as a safe and effective alternative for many men.
The latest innovation in focal therapy is a robotic device that enables more precise targeting of the prostate cancer cells.
This technology ablates targeted cancer tissue with heat generated by sound waves, while sparing healthy areas of the prostate.
Key benefits of this Hifu device are:
> Minimal or no treatment- related conditions
> Repeatable if necessary
> Does not exclude future radical treatments (i.e. surgery or radiation).
A recent British study showed that focal therapy is often more cost-effective than whole-gland treatment due to lower complication rates, shorter recovery time (often can be done as a day-care procedure), and reduced overall healthcare costs.
Despite its advantages, focal therapy is not yet universally adopted.
Key barriers include:
> Unsuitability for high-grade or multifocal cancers – such patients need whole gland treatment like radical prostatectomy or radiotherapy if the cancer is still localised
> The need for strict patient selection
> Dependence on high-quality imaging, which is not consistently available worldwide.
In summary
The way we understand and treat prostate cancer is undergoing a profound transformation.
With advanced diagnostic tools and innovative treatments like focal therapy, we now recognise that:
> Only about 15% of localised prostate cancers are aggressive and require radical treatment like surgery or radiotherapy
> The majority (85%) can be safely monitored or treated with focal therapy
> Prostate cancer can often be managed as a chronic condition, i.e. controlled over time while preserving quality of life.
The role of today’s urologist or oncologist extends beyond cancer eradication.
It includes guiding patients through their options, balancing survival outcomes with quality of life, and empowering them to make informed choices.
In short, prostate cancer is no longer always a disease to fear; increasingly, it is a disease that can be managed.
Datuk Dr Tan Hui Meng is a consultant urologist. For more information, email starhealth@thestar.com.my. The information provided is for educational and communication purposes only, and should not be considered as medical advice. The Star does not give any warranty on accuracy, completeness, functionality, usefulness or other assurances as to the content appearing in this article. The Star disclaims all responsibility for any losses, damage to property or personal injury suffered directly or indirectly from reliance on such information.





